
Newsroom
Innovative Drug-Delivery Nanoparticles Enhancing Glioblastoma Treatment Efficacy
Innovative peptide-coated nanoparticles offer a promising breakthrough in overcoming the blood-brain barrier to deliver targeted chemotherapy for glioblastoma, potentially transforming treatment outcomes for this aggressive brain cancer.
Challenges in Glioblastoma Treatment and Blood-Brain Barrier
Glioblastoma, an aggressive form of brain cancer, presents significant treatment challenges due to its high fatality rate. A major hurdle in managing this disease is that traditional chemotherapy drugs often struggle to penetrate the protective blood-brain barrier. The five-year survival rate remains below 10 percent despite surgery, radiation, and oral chemotherapy such as temozolomide.
Innovative Nanoparticle Drug Delivery Using Human Tissue Models
Researchers at MIT are pioneering the development of drug-carrying nanoparticles designed to enhance drug delivery to the brain more effectively than conventional methods. Their innovative approach utilizes a human tissue model that accurately mimics the blood-brain barrier, demonstrating the nanoparticles’ ability to infiltrate tumors and effectively kill glioblastoma cells.
To replicate the blood-brain barrier’s structure, Kamm’s lab has developed a microfluidic model using patient-derived glioblastoma cells and human endothelial cells to form blood vessels around the tumor cells. This model also incorporates pericytes and astrocytes, which are crucial for molecule transport across the barrier.
Surface Functionalization and Enhanced Penetration Mechanisms
Hammond’s lab introduced a technique known as layer-by-layer assembly to create surface-functionalized nanoparticles that encapsulate drugs. In this study, they coated nanoparticles with a peptide called AP2, previously shown to enhance transport across the blood-brain barrier. Testing these nanoparticles on glioblastoma and healthy brain tissue models revealed that AP2-coated particles significantly improved penetration through tumor-associated vessels.
Binding to a receptor named LRP1, which is more prevalent near tumors than in normal brain vessels, was identified as a key mechanism of this enhanced delivery.
“Peptide-coated nanoparticles led to increased tumor cell death compared to uncoated particles or free drugs, emphasizing the specificity of this approach.”
Preclinical Validation and Future Directions
The researchers loaded these nanoparticles with cisplatin, a standard chemotherapy agent. The peptide-coated nanoparticles were effective at targeting and killing glioblastoma cells within the tissue model, while non-coated particles harmed healthy blood vessels instead of focusing on tumors.
Subsequently, the team administered the nanoparticles to mice, using specialized surgical microscopes to monitor their movement within the brain. The results mirrored those observed in the human tissue model, demonstrating the particles’ capacity to cross the blood-brain barrier effectively.
Coated nanoparticles delivering cisplatin were found to slow tumor growth in mice, though results were less pronounced than in tissue models—likely due to the advanced stage of tumors in the animal studies. Future experiments aim to explore various drugs and nanoparticle formulations for enhanced efficacy and broader applications across different brain tumor types.
Expanding Research and Broader Impact
‘This model can help us design more effective nanoparticles,’ states Joelle Straehla, clinical investigator at MIT’s Koch Institute and pediatric oncologist at Dana-Farber Cancer Institute. ‘Although we’ve only investigated one type of brain tumor so far, our goal is to expand this research to include various other tumors, particularly rare forms that are challenging to study due to limited sample availability.’
The methodology for creating this brain tissue model has been detailed in a recent publication in Nature Protocols, enabling other laboratories to adopt this innovative approach.
This research was partially funded by several grants, including those from the National Cancer Institute and various cancer research initiatives aimed at improving treatment outcomes for patients with brain tumors.
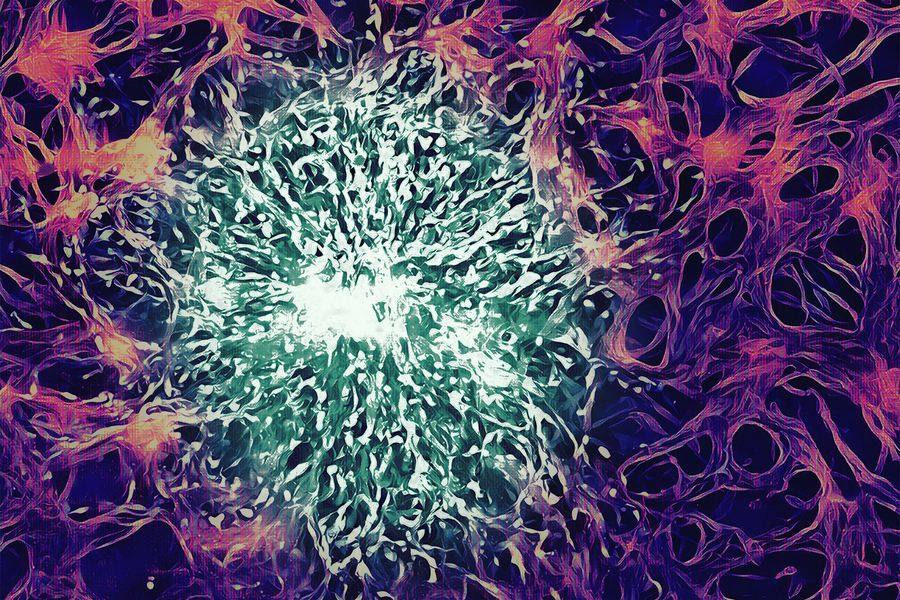
Image credit: Researchers at MIT developing nanoparticle therapies for glioblastoma



